Origin: ectoderm and neural tube
(I) Neural tube – previous notes
(II) Neural crest – Ectodermal cells on lateral edge of neural tube
Derivatives of neural crest:
- All dorsal root ganglia
- Autonomic ganglia
- Sensory ganglia of cranial nerves V, VII, IX, X (5, 7, 9, 10)
- Schwann cells
- Medulla of suprarenal gland (chromaffin cells)
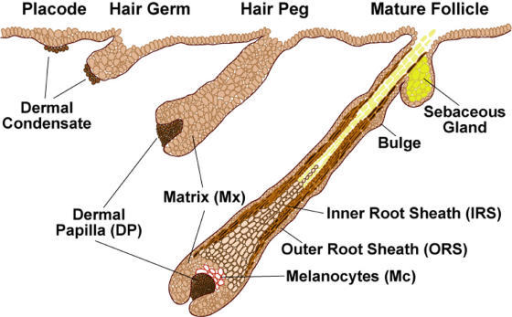
- Melanoblast cells
- Archnoid and pia mater
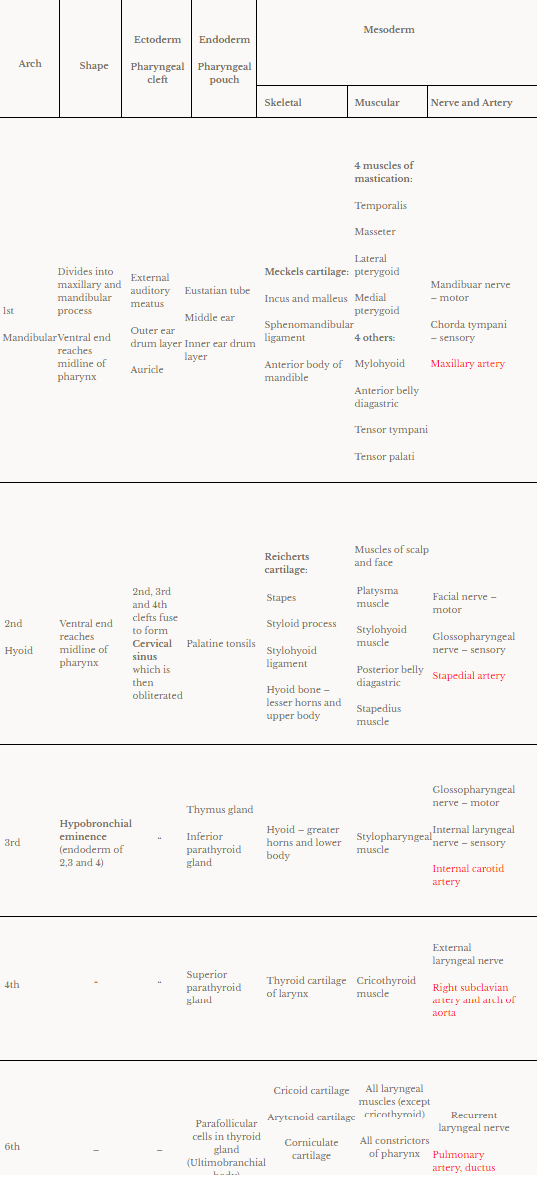
(III) Spinal cord – Caudal part of neural tube
- Neural tube has a single layer of simple columnar epithelium and central canal
- The epithelium proliferates – forms 3 layers:
- Ependymal layer – produces cerebrospinal fluid (CSF)
- Mantle layer – grey mater
- Marginal layer – white mater
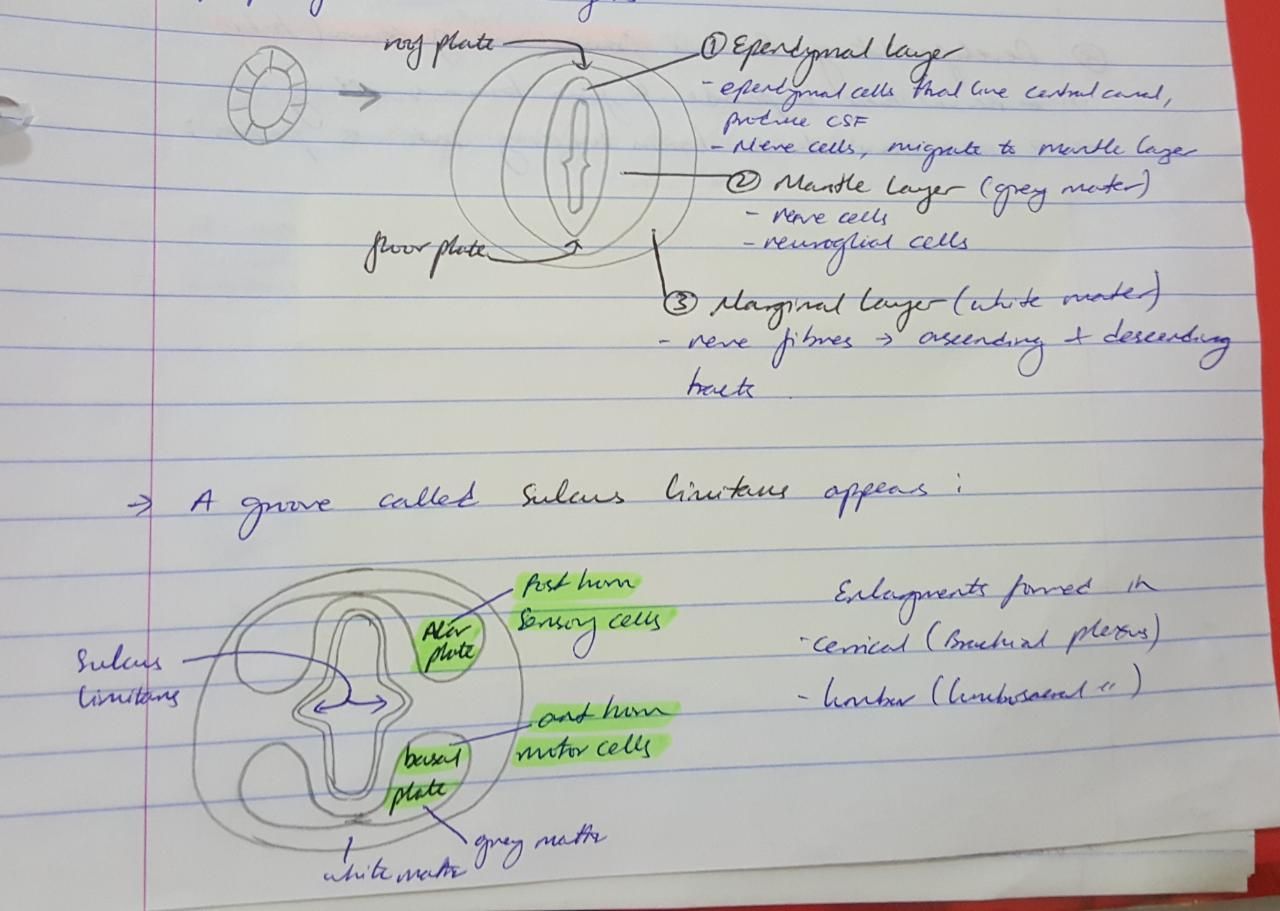
A groove called sulcus limitans divides the mantle layer into:
- Alar plate – posterior horn, sensory cells
- Basal plate – anterior horn, motor cells
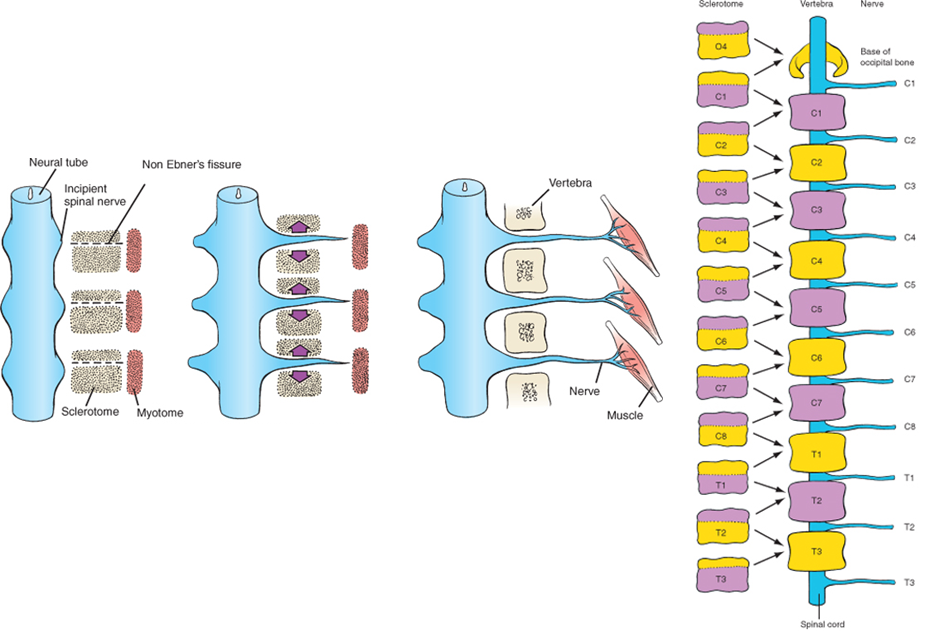
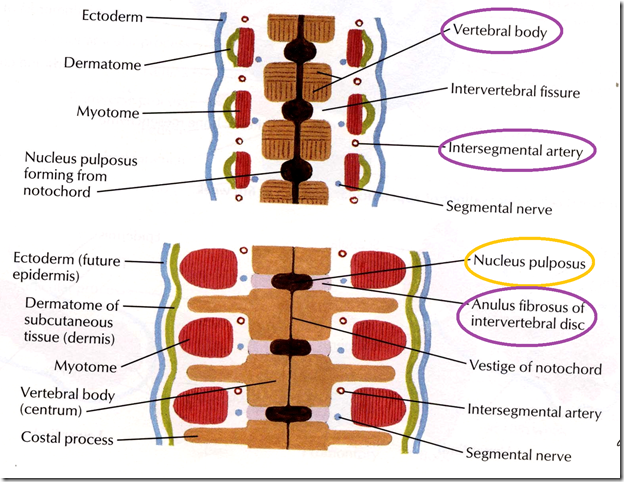
Growth of spinal cord:
- 3rd month fetal life – till end of vertebral column
- Birth – till L3
- Adult – till L1/L2
Congenital anomalies of spinal cord:
- Spina bifida oculta – failure of fusion of one vertebrae dorsal part
- Meningocele – failure of fusion of 2-3 vertebra. meninges bulge out
- Meningo-myelocele – spinal cord bulges out
- Myelocele – Neural tube failed to close, neural plate exposed


(IV) Brain – Cranial end of neural tube
- Neural tube expands to form brain swelling
- Lumen forms ventricles
- 2 constrictions divide brain swelling into 3 parts
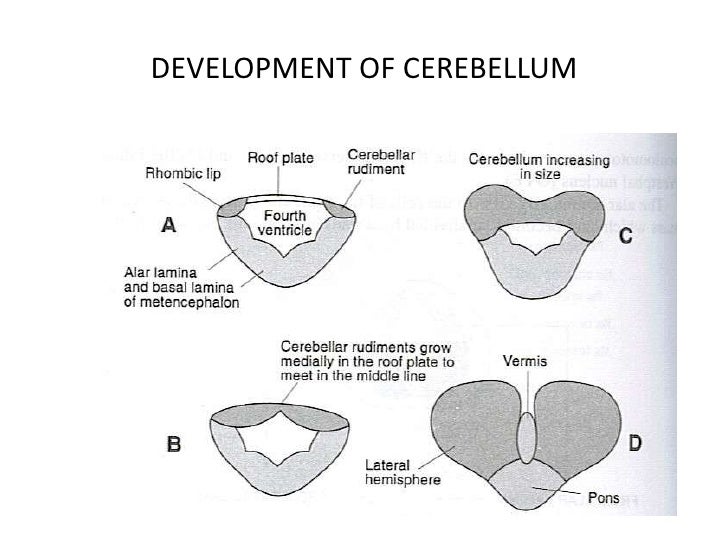
(V) Cerebellum – Alar lamina of metencephalon
- Alar lamina bend medially, forming medial and lateral bulges
- The medial bulges meet each other over the roof plate of 4th ventricle, forming vermis
- Lateral bulge forms cerebeller hemispheres
- Cerebeller cortex formed by – neuroblast cells migrating from mantle layer to marginal layer
- Dentate nucleus – neuroblasts deeply situated in mantle layer
- Cerebeller peduncles – axons of neurons of cerebeller nuclei grow out to reach brainstem