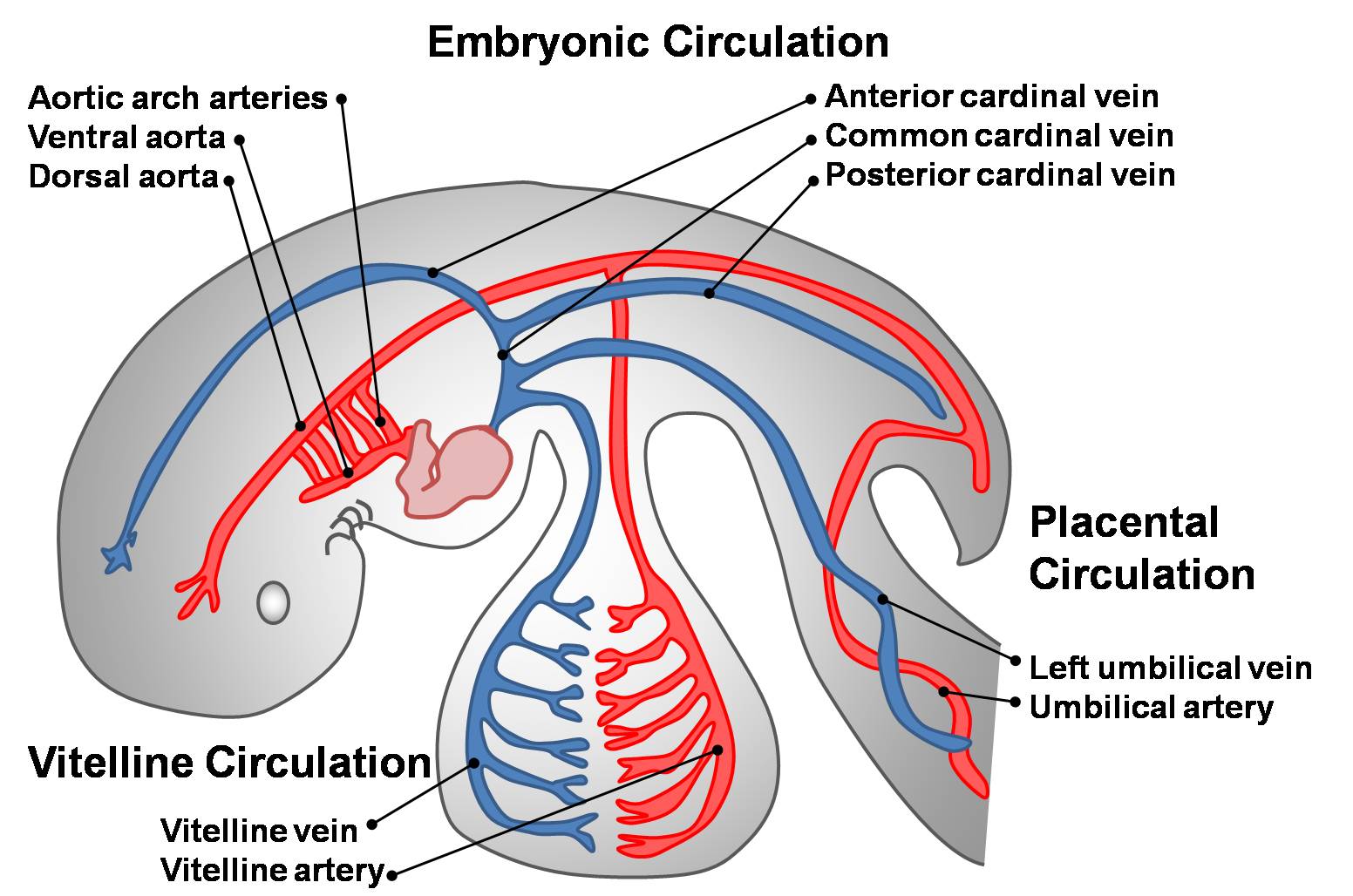
- Oxygenated blood
- ⇓
- Placenta
- ⇓
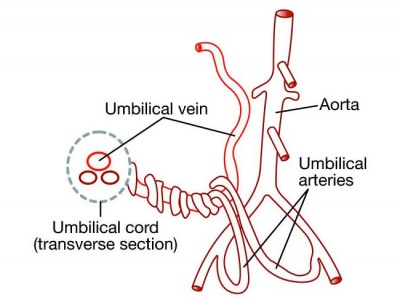
- Umbilical vein
- ⇓
- Through liver
- ⇓
- Ductus venosus
- ⇓
- IVC ⇐ Deoxygenated blood from lower limb
- ⇓
- Right atrium
- ⇓
- Foramen ovale (opening of IVC faces foramen ovale)
- ⇓
- Left atrium
- ⇓
- Left ventricle
- ⇓
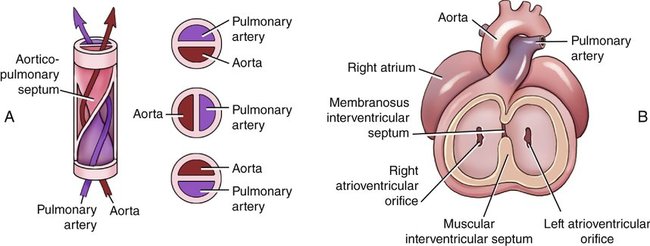
- Aorta which distributes blood
- Deoxygenated blood
- ⇓
- SVC
- ⇓
- Right atrium
- ⇓
- Right ventricle (septum secondum prevents from entering foramen ovale)
- ⇓
- Pulmonary trunk
- ⇓
- Ductus arteriosus
- ⇓
- Arch of aorta
- ⇓
- Mix with oxygenated blood
- ⇓
- Common iliac artery ⇒ External iliac artery (oxygenated blood to lower limbs)
- ⇓
- Internal iliac artery
- ⇓
- 2 Umbilical arteries
- ⇓
- Placenta
Mixing of oxygenated and deoxygenated blood in fetus:
- Liver – Umbilical vein (oxy) + Portal vein (deoxy)
- IVC – Ductus venosus(oxy) + Blood from lower limb (deoxy)
- Left atrium – Right atrium (oxy) + lung buds (deoxy)
- Dorsal aorta – via ductus arteriosus
Changes in circulation after birth
Immediate:
- Pulmonary circulation starts – lungs expand, negative pressure, air suctioned
- Closure of foramen ovale – Pressure increases in left atrium due to pulmonary circulation, therefore septum primum and septum secondum pushed together
- Closure of ductus arteriosus to form ligamentum arteriosum. From pulmonary trunk to arch of aorta
Late:
- Ductus venosus forms ligamentum venosum of liver. From left portal vein to IVC
- Umbilical vein – ligamentum teres of liver. From umbilicus to left portal vein
- Umbilical artery – Lateral umbilical ligament. From superior vesical artery to urinary bladder.